Scleroderma
Scleroderma is a rare autoimmune condition causing the overproduction of collagen in the body.
Scleroderma, Explained
Dr. Collene Marizza Galeng, a Board-Certified Rheumatologist, gives a brief overview of Scleroderma in this short explainer video.

What is Scleroderma?
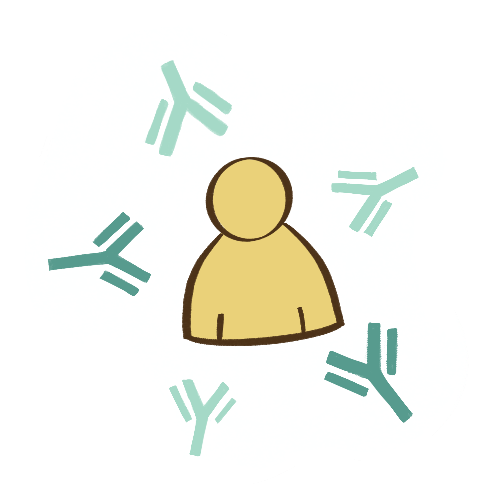
The immune system is responsible for protecting the body from infections or diseases. In a person with Scleroderma, the body’s immune system abnormally attacks the body, causing high amounts of collagen to build up in body tissues, leading to stiffness or hardening. Scleroderma is rare and lifelong, and in some cases, it may affect several organs over time.

What can cause Scleroderma?
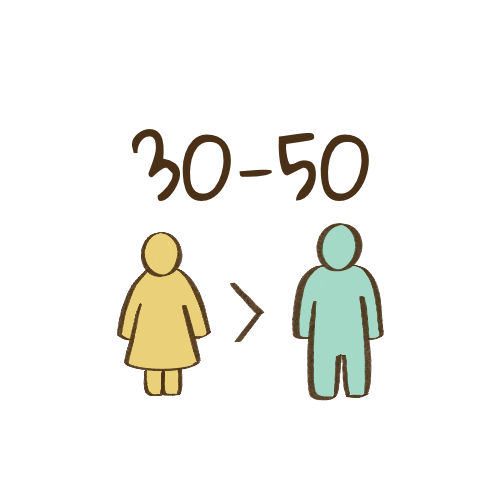
The causes of Scleroderma are not fully understood. However, it is believed that a person becomes at risk of developing the disease through the passing of genes associated with autoimmunity. Like other autoimmune diseases, it is most likely to occur in females.
Having the genes for Scleroderma can make a person more prone to develop the disease through certain triggers. While the exact triggers are unknown, some sources point to certain viruses, stress and exposure to chemicals such as silica and organic solvents.
Scleroderma affects lives, and knowing about it can help build support for persons who have the disease.

Scleroderma affects lives, and knowing about it can help build support for persons who have the disease.

Localized
Systemic
What are possible symptoms of Scleroderma?
There are two kinds of Scleroderma – localized and systemic. Localized Scleroderma is most common, affecting primarily the skin. On the other hand, Systemic Scleroderma affects the skin and internal organs. Systemic Scleroderma can be further divided into the limited type and the diffuse type, which can be differentiated by the area where skin changes are seen, symptoms, and laboratory test results.
Skin changes are the most visible signs in a person with Scleroderma. The disease may be difficult to recognize because its symptoms may be similar with other diseases. However, a combination of symptoms can point to the possibility of having the condition. The card section below shows possible signs and symptoms of Scleroderma. Keep in mind that these may occur in different stages of the disease.

Click on a symptom card to learn more.

Raynaud's Phenomenon

Finger Pitting or Ulcers

Teleangiectasia or Spider Veins

Swelling of Hands

Skin Thickening

Salt and Pepper Skin
Joint Pains

Movement limitations
Small Mouth Opening

Digestive Problems

Difficulty Breathing

Arrhythmia or Abnormal Heartbeat

High Blood Pressure

How will I know if I have Scleroderma?
The diagnosis of Scleroderma is confirmed through physical symptoms and specific laboratory tests. These tests typically require the extraction of blood to check for specific antibodies. Other baseline exams may also be requested to check for internal organ involvement.
Early diagnosis is very important for persons with Scleroderma. If you know someone who is experiencing the symptoms mentioned above, it is encouraged that they seek consult with a Board-Certified Rheumatologist.
Click the button below to be directed to the Philippine Rheumatology Association website, where you can find a rheumatologist near you.
Note: This will take you out of the Beyond Scleroderma website.





Is there a cure for Scleroderma?
There is currently no cure for Scleroderma, but it can be controlled. Treating Scleroderma involves taking prescribed medications and following lifestyle changes that relieve symptoms and slow disease progression. Patients may also experience periods called remission, where one may feel generally well, as if without the disease.
Regardless, it is important to maintain regular check ups and to follow the doctor’s advice. Self-medication with other medications, herbal treatments, or alternative medicine is also discouraged as it may cause harm to patients.





© BEYOND SCLERODERMA, 2025
CONTACT US
De La Salle-College of Saint Benilde, Design and Arts Campus (D+A Campus)
scleroderma.benilde.mma@gmail.com
© BEYOND SCLERODERMA, 2025
CONTACT US
De La Salle-College of Saint Benilde, Design and Arts Campus (D+A Campus)
scleroderma.benilde.mma@gmail.com
Developed and designed by: Arnante | Bautista | Sua